After urostomy surgeryYou will be wearing a urostomy bag, which will most likely be transparent or have a viewing window, so that your nurses can check on the colour and size of your stoma easily. A night drainage bag will be attached to collect your urine at first.
After surgery, you will have some thin tubes called stents coming out from your urostomy. The purpose of the stents is to protect the newly formed join where the ureters meet the piece of small bowel. The stents may fall out by themselves, but if they don’t your Stomal Therapy Nurse will gently remove them, once the initial post-operative swelling has started to Looking after your urostomy can be a bit fiddly until this time, but management will feel easier once they are removed.
After your operation, you may experience some constipation. It is normal for there to be some disruption to your bowel movements following this procedure as a result of using part of your small bowel to create your urostomy, and also because your usual pattern of eating and drinking has been disrupted. Once your bowels start to work again, you may experience diarrhoea for a short while, but this will pass and gradually things should settle.
|
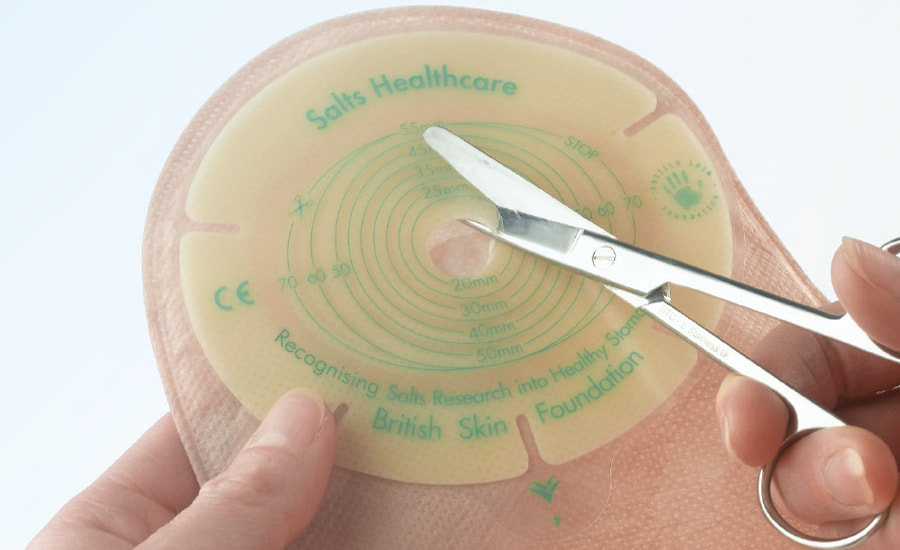
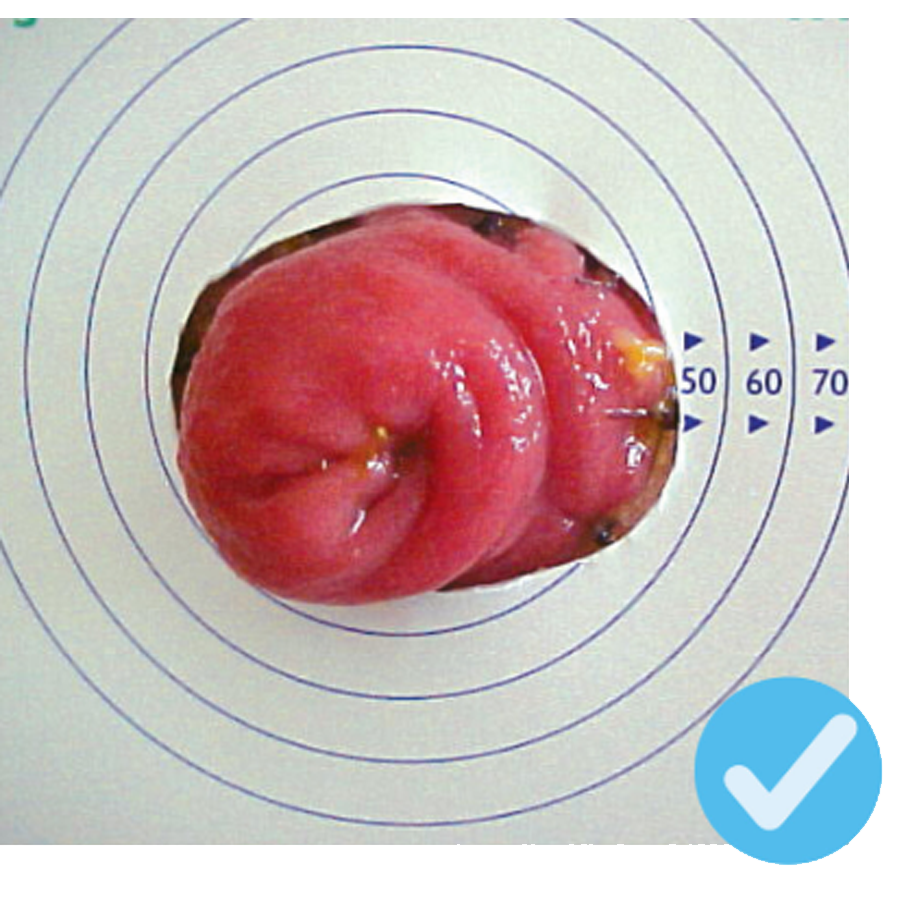
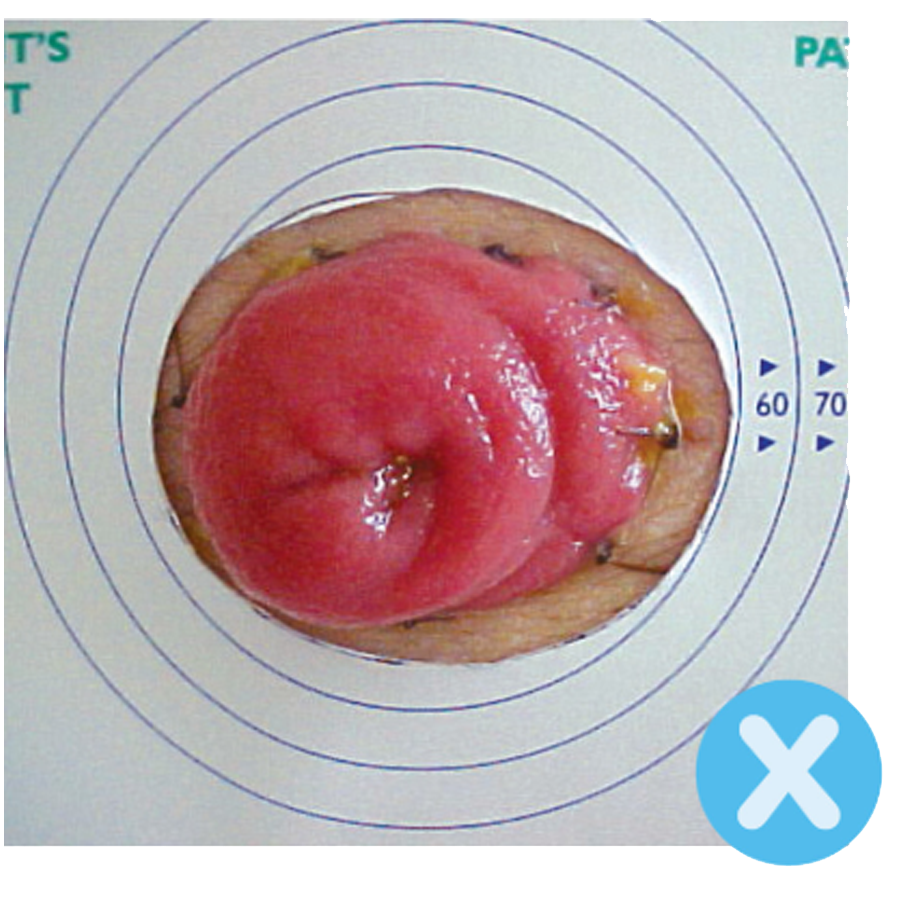
Urostomy Bag - front and back
|